Editor’s Note: This is the second installment of our three-part series based on a new, independent research study called Partnering for a Healthier America. As the opioid crisis continues to take lives, there is more work to be done within the healthcare industry to help reverse the path we are on today. This series provides new information that can help the health industry address the unique challenges of this crisis.
Acute and chronic pain are at the center of much of the current opioid crisis. Nearly half (46%) of those who responded to our survey suffer from musculoskeletal pain which includes back pain. Back pain is the predominant condition followed by osteoarthritis (33%), nerve pain (22%), chronic headaches (21%) and a multitude of other disorders.
During Escalent’s recent national study looking at America’s opioid crisis, we asked respondents about their relationship with pain. Our Health team found that more than one-quarter (28%) of all respondents suffer from some form of chronic pain. The study also found that the pain is constant and long-lasting—61% say that they experience pain every day, and half have been in pain for at least five years.
I’ll admit that I used to be skeptical of those who complained of chronic pain and deferred to prescriptions to manage it. But over the last year, after physical trauma, ongoing stress, less-than-stellar posture and inadequate exercise, I developed chronic lower back pain. I had hoped that my pain would be relieved with visits to my chiropractor, but nine months later the pain is still present.
While I have not sought out prescriptions to manage the pain, I now admit I understand the desire to do so. I am beyond busy with a demanding career and raising two young children, so taking time out of my day to see any kind of therapist or practitioner is difficult, and the out-of-pocket expenses for office visits add up quickly. Taking a prescription medication would be less burdensome overall, cheaper and provide instant relief (though short-lived). Yet, I am concerned about prolonged medication use in regards to side-effects and of course, the addictive properties, along with knowing the medicine is just masking symptoms and not addressing the underlying reason for my pain.
Through my own experience, I have a new respect for the challenges that those with chronic pain face, and through this study, I have developed a better understanding of some of the obstacles the healthcare industry faces in managing chronic pain without resorting to prescriptions, a pattern that is feeding into the opioid epidemic.
The problematic convenience of opioids
Affordable, effective and easy to administer, the benefits of opioids for the medical sector are clear, so it is no surprise to see in our study that opioids are by far the most commonly prescribed medications—with Hydrocodone, Tramadol, Codeine and Oxycodone cited as four of the top six prescriptions.
For patients, it’s also easy to see the appeal of prescription painkillers. Immediate pain relief doesn’t take a lot of time out of your schedule, and it is generally cost-effective. Which brings us to our next question in this healthcare insurance market research: what are the alternatives? And why aren’t doctors recommending them? And why aren’t patients adopting them?
Exploring opioid alternatives
Interestingly, we found that most people (82%) suffering from chronic pain are at least somewhat likely—and nearly two-thirds are extremely likely—to consider a non-prescription alternative if it had the same efficacy as their current prescription. Over two-thirds also say they would even consider a less effective alternative.
So, what’s stopping them?
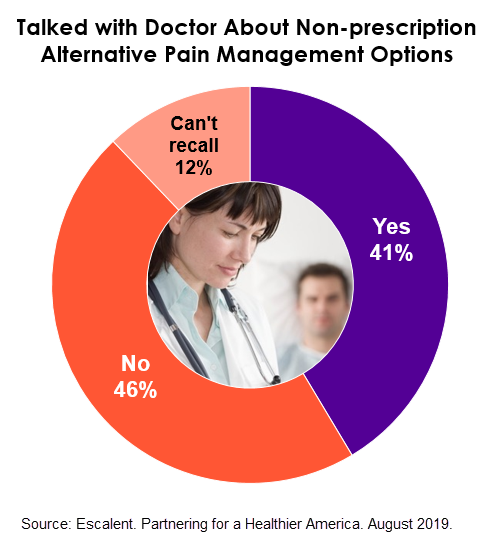
Perhaps one of the most surprising healthcare insurance market research findings in our study is that among those who experience chronic pain, well over half (58%) say that either their doctor has not spoken with them about prescription alternatives or they don’t recall their doctor having done so.
While there will always be people with pain for whom opioids seem to be the only relief that works, there are those who could possibly manage pain without opioids. So why aren’t more doctors recommending other modalities?
- Physician visits are short—a scant 20 minutes is hardly enough time to effectively learn the patient’s issue and explain one option, let alone cover a range of options that may be more complicated than taking a pill.
- Physicians feel a tension in upholding their promise to first do no harm—is it more harmful to let a patient suffer pain, or to risk addiction?
- Physicians are facing increasing pressure to maintain patient satisfaction scores, and denial of certain medications, even when not medically necessary, has the potential to decrease the patient’s satisfaction with the doctor’s services.
- When other treatment options are discussed, there are often obstacles beyond the control of the physician (such as the alternate treatment not being affordable or covered by insurance).
As for patients, lack of awareness and low doctor recommendation, as we see in the data, are likely the key drivers of lower use of alternative pain management. Currently, while there might be some coverage for non-prescription alternatives to pain management, it is covered differently—usually with frequent out-of-pocket costs such as practitioner copays, or with a capped number of visits within a year. This, in turn, encourages patients to default to using inexpensive and convenient drugs to alleviate the pain. As a result, doctors likely face an obstacle in getting a patient to try a non-prescription alternative, even if they feel an alternative therapy may work for their patient.
Forging a partnership between carriers and providers
With increasing focus on America’s opioid epidemic, more and more people are looking to the healthcare industry to help tackle the problem at its source.
In 2017, the Department of Health and Human Services (HHS), as part of its strategy for combating the epidemic, outlined how they will work with the healthcare system to advance better practices for pain management. Specifically, HHS claimed, “We are committed to going through all of the important work HHS does—in payments, prescribing guidelines, and more—to ensure that we are not pushing doctors toward quick fixes that risk lives. Our goal, in all that we do, should be to promote healthy, evidence-based ways of managing pain and to help providers and patients make responsible choices.”
In other words, HHS has made it clear that a whole-system approach would be necessary for solving this problem and acknowledged that a solution starts not with addiction treatment but at the outset of the cycle—with better pain management—which requires a joint effort from insurers and providers.
Surprisingly, consumers are also looking to insurance companies for guidance. Our research shows that people are just as likely to consider alternative forms of treatment if they are recommended by an insurance company as they are to consider those based on a doctor’s recommendation.
This has major implications for insurance companies seeking to influence this space, as there is not only pressure from the government to act, but also an appetite from consumers to listen to insurers’ recommendations. That’s why an increasing number of insurance companies have begun to explore ways they can work with providers to make alternatives easier to offer and more affordable for patients.
Partnering for a Healthier America is a valuable tool for insurers that want to better understand their role within the current opioid crisis that is gripping America. Crucially, it also gives direction to help insurers collaborate with physicians to provide better coverage for non-opioid pain management options.
Download your copy of Partnering for a Healthier America and stay tuned for the final installment of our series exploring America’s opioid crisis.