
Editor’s Note: This is the first installment of our three-part series based on a new, independent research study called Partnering for a Healthier America. As the opioid crisis continues to take lives, there is more work to be done within the healthcare industry to help reverse the path we are on today. This series provides new information that can help insurers and health systems address the unique challenges of this crisis.
Insurance carriers, among other healthcare sectors, are increasingly approaching Escalent’s Health team to help them develop strategies to address the opioid crisis—research that looks at consumer attitudes and preferences for pain treatment options as well as maps out the lives and broader context of people who experience chronic pain and/or use opioid prescriptions. Insurance companies, in turn, are being approached by their employer customers for help in understanding and addressing the issue within specific employee populations.
In response, Escalent conducted a nationwide study of 972 US adults in August 2018 to help insurers better understand consumers’ preferences, attitudes and behaviors around pain management to pinpoint areas of opportunity to improve their services or coverage for pain management.
Do insurance companies have a responsibility to help solve this problem?
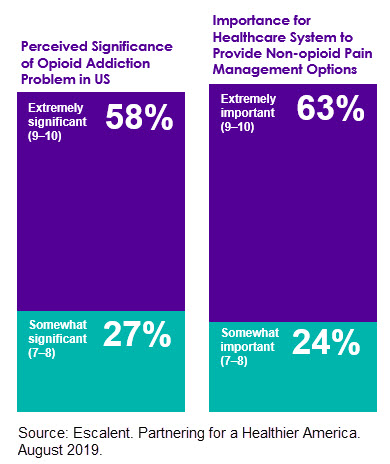
According to our research, over half (58%) of US adults consider opioid addiction to be an extremely significant problem, and nearly two-thirds (63%) say it is “extremely important” for the healthcare industry to be involved in solving the problem.
Insurance companies may face a dilemma in helping to solve this problem when there are obvious trade-offs between cost or efficiency and health risks. Opioids are generally inexpensive to cover and easy to provide, while alternative pain treatments may be costlier at the outset even if they result in long-term savings, and research on the efficacy of non-opioid pain treatments is lacking.
However, with a higher level of attention on this crisis, all stakeholders in the healthcare industry need to consider their own responsibilities to the public relative to this crisis. And insurance carriers have taken note, with several well-known carriers publicly committing to work on the problem. A late 2018 press release claims that Cigna has met its goal of 25% opioid-use reduction among its member population ahead of schedule. Aetna, UnitedHealthcare and Blue Cross Blue Shield have developed agendas and task forces to address the situation.
Where do insurers go from here?
It’s vital that insurers develop strategies to address the opioid crisis, but those strategies need to be informed by the consumer. Continue reading this series to find out what we’ve learned about those who experience chronic pain, what they are willing to do to address it, and how insurance companies and providers can help provide access to better options.
Download your copy of Partnering for a Healthier America and stay tuned for future installments of our series exploring America’s opioid crisis.








