Editor’s Note: This is the final installment of our three-part series based on a new, independent research study called Partnering for a Healthier America. As the opioid crisis continues to take lives, there is more work to be done within the healthcare industry to help reverse the path we are on today. This series provides new information that can help insurers and health systems address the unique challenges of this crisis.
We know the opioid crisis is impacting millions of Americans every year and claiming the lives of tens of thousands of people. The first article in the series provided contextual understanding of the opioid crisis in the US, and the second article outlined the obstacles that are keeping us from effectively treating pain. This article explores alternative treatment options and how we can knock down barriers to access other forms of pain management.
Alongside the human cost, the impact of the opioid crisis is also taking a toll on every area of the medical sector. Research suggests it has caused reductions of $26 billion in federal tax revenue and $11.8 billion in state tax revenue between 2010 and 2016, staggering figures that represent just the tip of the iceberg in terms of the epidemic’s financial toll. Given these numbers, why haven’t we explored the use of alternative treatments for pain management, many of which are less expensive and, in some cases, more effective in the long term?
Consumers need better access to alternatives
Our study found that doctors are primarily going straight to prescriptions to help patients manage their pain. However, we also found that 82% of respondents are willing to consider a non-prescription alternative. And, while it is true that those with chronic pain are trying multiple modalities, it is somewhat surprising that many methods identified as being more effective in medical research don’t appear highly on the list of what consumers currently use. Only 2% say they currently use acupuncture, and biofeedback therapy receives no mention at all. It seems that certain approaches may need stronger recommendations from providers in order to increase patient awareness of the options. Meanwhile, insurers should review coverage of these high-efficacy approaches together with messaging about alternatives sent to members.
Those with chronic pain are primarily using over-the-counter and prescription medications (61% and 49%, respectively). After medications, top-used modalities include exercise (31%), physical therapy (17%), surgical or injection procedures (15%), transcutaneous electrical nerve stimulation (TENS) units (14%), mindfulness/meditation (14%), massage therapy (13%) and marijuana (12%).
While we generally don’t dispute the benefits of exercise, physical therapy, surgical or injection procedures, TENS units, meditation and massage, what about marijuana? Though decriminalization of the drug began in the mid-1970s, only recently has the legalization of marijuana begun to gain significant traction. To date, 11 states have legalized marijuana for recreational use and 35 have legalized medical marijuana use.
Is marijuana a viable alternative?
Given its recent legalization in areas across the country, could marijuana provide a safe, effective and affordable alternative to opioids? Some recent studies support the need to further explore marijuana as an effective alternative:
- The Journal of Psychoactive Drugs published a study in 2019 that found a significant reduction of opioid use for pain relief when using marijuana.
- The American Journal of Psychiatry published a study in 2019 that found use of cannabidiol (CBD) was an effective treatment to reduce cravings for and help break addiction to opioids.
- The Journal of General Internal Medicine found that “in states where marijuana is available through medical channels, a modestly lower rate of opioid and high-risk opioid prescribing was observed.”
However, other studies show there is more work to be done when it comes to using marijuana in place of opioids. Most specifically, a new study by PNAS indicates that substituting cannabis for opioid may not be directly linked to lower deaths as reported in 2014.
Marijuana is certainly not a cure-all for every chronic pain condition; the clinical research on its use as a pain management technique is still in its infancy, and some studies show that marijuana has a narrow therapeutic window for pain management. However, epidemiological studies do show initial evidence that marijuana use reduces reliance on opioid pharmacotherapy.
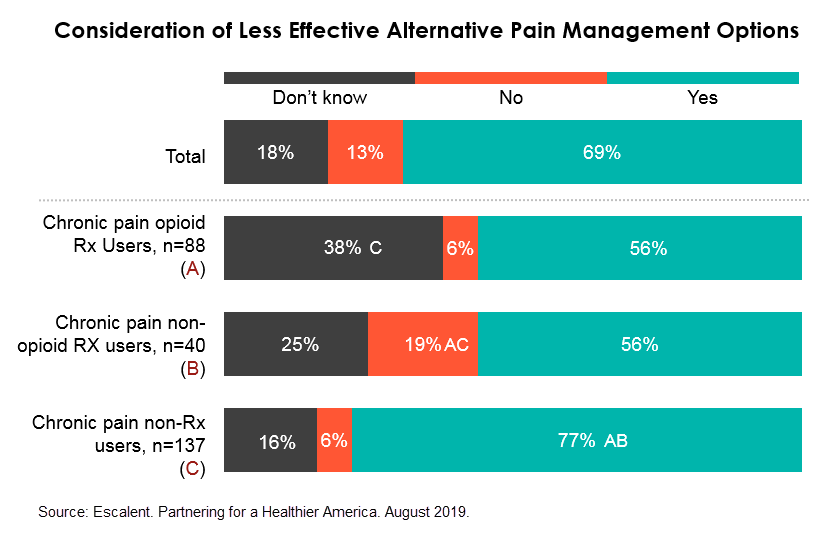
Our study suggests that marijuana has a role to play; over half (56%) of those with chronic pain say they would consider alternative pain management options even if less effective than prescriptions, meaning that marijuana’s narrow therapeutic window may be an acceptable trade-off. And among those who only use prescription medications to manage pain, marijuana was the third-preferred option after physical and massage therapy. Additionally, prescription-only users would even prefer using marijuana to over-the-counter medications.
What is next for insurers?
Clearly, healthcare providers need to adjust their approach to provide support for alternative pain management techniques if they expect to combat the opioid crisis, reduce its overall strain on the healthcare system, and improve the quality of life for a substantial portion of the population.
Insurers have a significant role to play in that, too. Investigating and understanding provider and member needs, perceptions and behaviors will be important to create programs that raise awareness and education on alternatives. In addition, providing more coverage for a broad array of alternatives, including medical marijuana, by breaking down barriers to access other forms of pain management will be a positive step toward evolving the medical system to better treat pain for the benefit of the patient.
Partnering for a Healthier America is a valuable tool for insurers that want to better understand their role within the current opioid crisis that is gripping America. Our health study provides direction for providing better coverage for non-opioid pain management options and identifies opportunities for working with healthcare providers to better communicate alternative pain management programs.