As the Popularity of Telehealth Grows, Some Barriers Continue to Nag the Industry
Across every industry, COVID-19 has highlighted the opportunities technology presents in times of crisis. For the healthcare industry, all eyes are on telehealth.
Articles touting the virtues and potential industry-altering impact of telehealth ramped up in the early days of the pandemic. Telehealth gives patients the option to receive healthcare treatment and/or advice using live video via smartphones, laptops or tablets, and minimizes the need for patients to travel to their provider’s office.
Over the years, the American Medical Association (AMA) has found that more primary care physicians are seeing the value of digital tools to deliver quality healthcare, including virtual visits, remote monitoring for efficiency, clinical decision support and patient engagement.
Not only does telehealth enable patients to avoid crowded waiting rooms that could contribute to the spread of COVID-19, but patients save time traveling to an office and may seek treatment for conditions they are uncomfortable seeing a doctor for in person. As concerns for COVID-19 grew, many predicted that the circumstances would catapult telehealth to new, industry-altering levels.
“This is telehealth’s moment to shine,” said Rafid Fadul, MD, chief medical officer for telehealth company Wheel, as reported by Managed Healthcare Executive.
Is Telehealth Changing the Healthcare Industry?
Escalent’s Health team decided to put the theory of a telehealth-driven revolution for the healthcare industry to the test. We conducted a self-funded study to discover whether the healthcare industry was really changing.
Among the 1,381 people age 18 and over who completed our survey covering a variety of COVID-19-related topics, 14% used telehealth before the pandemic and 22% used it for the first time during the pandemic.
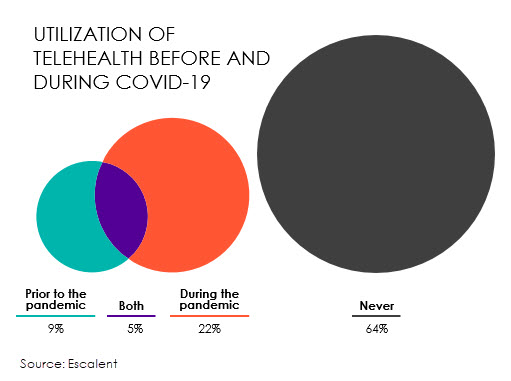
While we’re definitely seeing growth, telehealth remains an untapped resource for two-thirds (64%) of patients. With more patients now using telehealth, we wanted to know why we aren’t seeing a much larger boost in participation. This blog post shares the biggest barriers to telehealth and how you can give patients the peace of mind and confidence needed to consider telehealth as a viable option for their healthcare needs.
Understanding How Telehealth Fits In
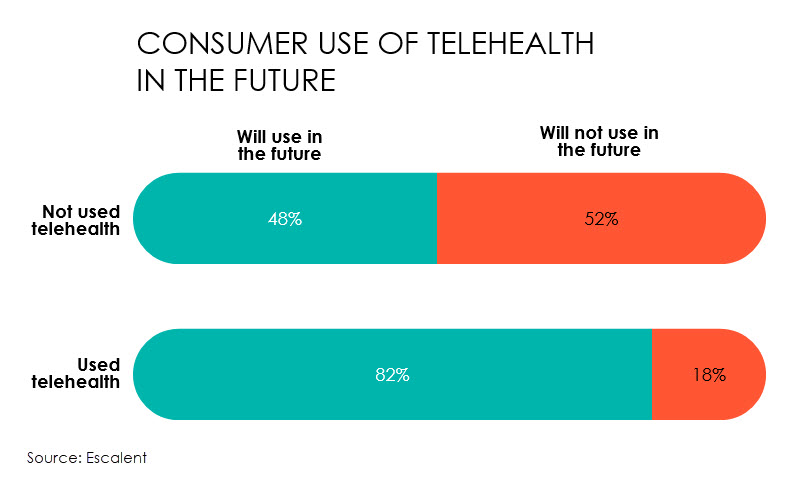
There are many reasons patients may not have tried telehealth yet—for instance, they simply might not have needed medical care during this time, or they may have been unaware that this type of care is available to them. The good news is the majority (82%) of those who have already used telehealth anticipate using it again, and more than half who have not used it yet are open to it.
Nonetheless, just under half of patients who have not used telehealth say they don’t expect to ever use it—this translates to about one-third of the population. In order for telehealth to grow, providers need to increase awareness, educating patients on what telehealth is best used for and how it can be relevant to them.
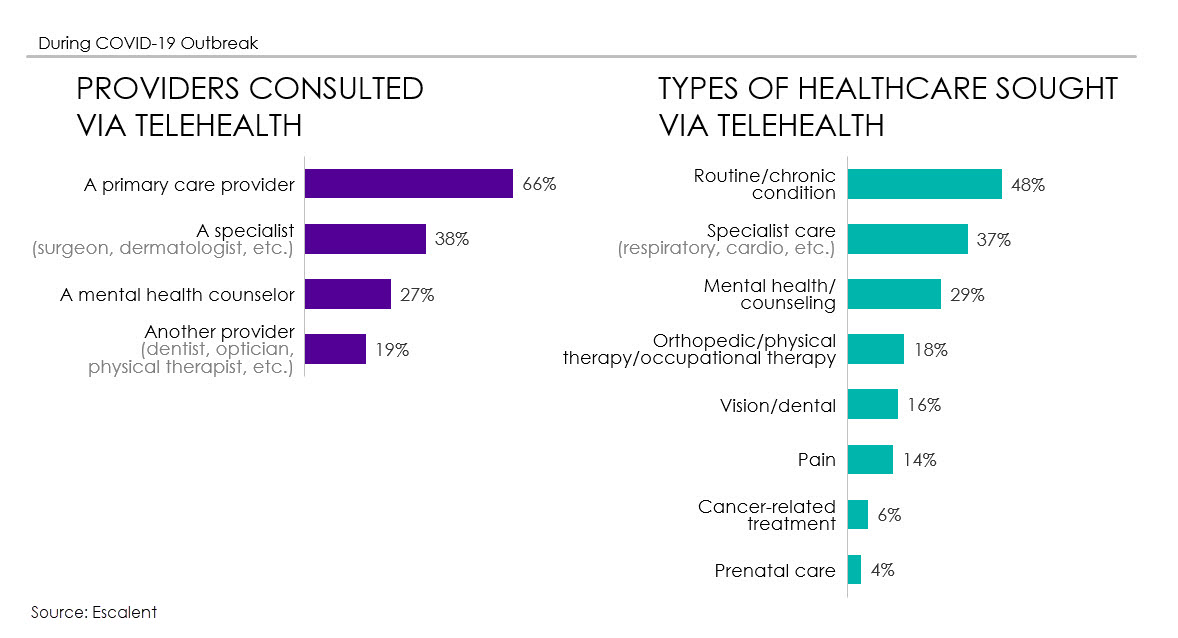
Patients can see their primary care doctor for a range of conditions—from allergies and infections to sore throats and sports injuries. Patients may also receive counseling from mental health and other specialists, or discuss lab results via videoconference.
Telehealth is also effective in helping patients develop stronger relationships with their doctors through more frequent meetings or check-ins. After lockdown restrictions are lifted, it will be important to let patients know that telehealth visits are not expected to replace all in-person visits but instead to supplement in-person care. This will ultimately provide patients with more high-quality care overall.
How People Have Used Telehealth During the Pandemic
The following chart shows the types of healthcare and providers patients sought via telehealth during the pandemic. This provides a view into the types of care that may be best suited for telehealth.
Not only is it important to understand how patients are using telehealth, but providers also need to know why so many patients who have not used telehealth are rejecting it as a possible future care option.
What Is Keeping People from Using Telehealth?
Our research shows that a preference for face-to-face interactions and concerns over quality of care or inaccurate diagnoses are the top reasons more patients have not used telehealth. These patients are more concerned about the things they may lose by using telehealth rather than about practical barriers, such as lack of at-home tools to assess vitals or lack of technical savvy.
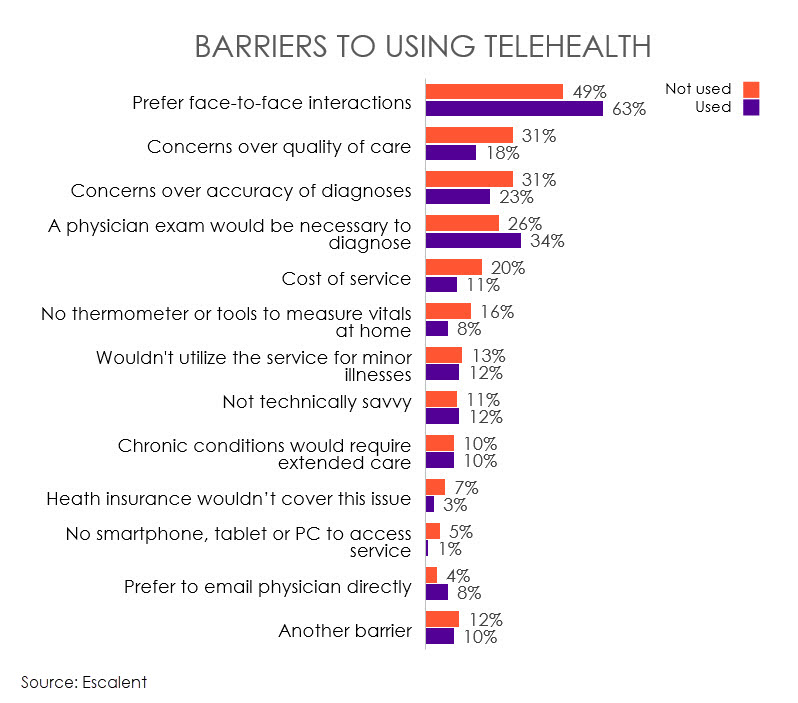
For the few users who don’t plan to use telehealth again, the primary barrier is also a preference for face-to-face interactions. Interestingly, among those who have tried telehealth, the concern over quality of care is reduced, suggesting that providers were able to meet basic needs for medical care during virtual interactions.
The big takeaway is that patients who don’t want to try telehealth prefer more personal contact with doctors. And if their first telehealth visit doesn’t go well, that lack of personal contact will likely be the main reason for never returning. Of course, there will always be people who prefer (or require) in-person visits, yet efforts to make the visit feel more personal will help make telehealth more acceptable to patients, especially during unpredictable times.
Improving the Reputation of Telehealth
About one-third of patients have not—and do not—anticipate using telehealth. So, how can providers, insurers and pharmaceutical manufacturers drive demand?
Here’s what we recommend:
- Assure patients of personal connection and quality care: Assuring patients that they will still be able to make a personal connection with a healthcare provider and receive quality care through a virtual visit is paramount to uptake. Frequent communication confirming that the in-person element will not be lost is key, and providers should find ways to back this up. For example, providers can provide anonymized testimonials on their website that show hesitant patients that these visits can still feel personal.
- Tell patients what to expect: Messaging that addresses what patients can expect during a telehealth visit can go a long way to put them at ease. For example, explain how healthcare providers diagnose or recommend treatment when they’re not physically in the room with the patient. Outline which tools patients will need, and what to do if the tools are not available. And assure patients that they can ask questions just as they would if they were in the office.
- Explain how telehealth fits with patients’ overall healthcare needs: Elaborate on how telehealth can work in conjunction with in-person visits to improve the care patients are already getting. Providers should emphasize the situations or medical concerns where telehealth works best, setting expectations so they can deliver care with higher levels of satisfaction.
- Personalize the messaging: Develop an outreach strategy for patients based on how best to care for specific conditions. For example, for patients with a chronic condition, let them know which aspects of their particular condition can be managed through telehealth versus in-person visits.
Strategic Summary
Telehealth might not be suitable for all patients and medical concerns, but the pandemic has highlighted the importance of telehealth as a viable care option. And while some people may not go back to telehealth when restrictions lift, the rise in use during the pandemic highlights the need to clarify when this healthcare option is best used, and the importance of overcoming persistent barriers.
In times of crisis and beyond, strategic messaging for reluctant patients will likely encourage them to consider all available resources—including telehealth—in managing their healthcare needs.
If you need help developing your brand’s message around the benefits of telehealth, both during and after the pandemic, send us a note.