
Where some industries have the benefit of conducting ethnographic or observational research to gain insight into key conversations or decision-making moments, this is not always the case in healthcare. With most of my research in pharmaceuticals, it can be difficult to gain access to some of the most important conversations to learn from, because they happen behind exam room doors, and rightly so—patient privacy is top industry priority. Because of the challenge—and the inherent desire to learn from those “closed door” conversations—I’m pleased to share how role-play allows Escalent’s Health team to unlock those insights for our clients!
When the gold standard is out of reach…
The gold standard for real-world insights is immersive, ethnographic research. I fully agree, and I’m incredibly grateful for the opportunities I’ve had to conduct immersive research with physicians in their practices and patients in their homes. However, there can be significant barriers that limit our abilities to conduct this style of research—particularly when our goals are to understand a specific decision or conversation that takes place in the journey of a disease state.
- Logistical hurdles: The coordination of finding patients and physicians at the right points in time and being able to secure consent from all parties can certainly be done—but it often takes time that our clients simply do not have, or exceeds the budgets that would be reasonable.
- Regulations and privacy: The increasing protections of patient privacy are an essential component of today’s healthcare system but create significant limitations for researchers seeking access to capture photography or video within physician practices. Added to that, while we may secure a physician’s and patient’s consent to in-situ research, securing institutional permissions to access the practice are an entirely different challenge.
- Ethical considerations: Having spent the last few years focused heavily in oncology business decisions, certain conversations deserve to remain sacrosanct between a patient and their physician. The moment a patient receives a metastatic cancer diagnosis and is being explained their treatment plan, is certainly a time where they deserve the privacy to react, emote, question and process—without additional eyes on them.
How can you achieve immersive learning without actual immersion?
The answer is simple—simulation. As a moderator, I simulate conversations with physicians frequently in the context of in-depth interviews. “Doctor, I’d like you to speak to me as if I were your patient and you were explaining this product to me.” It is an effective tool—except that the physician’s response is typically the abbreviated version, lasting about 45 seconds for a conversation that we know often takes close to 30 minutes.
Role-play, as a research tool, takes the same idea but immerses respondents in the full context of the conversation. The research team provides context, a simulated environment, a prepared actor—and we ask respondents to engage in a given conversation as they would in the real world.
You may be surprised to learn how comfortable physicians are with role-play; in fact, it’s a core part of their medical training. Given that they speak with patients every day, placing them in a scenario to have a natural, reflexive conversation reveals more truth than asking them to recount such conversations artificially.
Role-play is an especially valuable methodology when the core research objectives seek to understand a specific conversation, interaction or decision-making process. Where we might have preferred ethnographic or in-situ observation, role-play provides a time- and cost-efficient alternative that yields similarly rich insights. Specific objectives that are a great fit for role-play include:
- Understanding language or dialogue around a topic or product
- Exploring decision-making or recommendations in the moment
- Exploring how specific variables may shift decisions or conversation
To help bring this idea to life, I’ll set the scene: One of our clients, a global pharmaceutical company, was preparing for the launch of a first-in-class oncology treatment indicated for an advanced tumor. When approved, this product would change the existing treatment paradigm as an addition to the current standard of care and, ultimately, change the nature of treatment conversations that physicians would have with patients.
The Challenge
Our client was keen to understand the dynamics and dialogue of today’s current treatment conversations. Because their product would be indicated as an additional adjuvant therapy, our client needed to ensure that their product’s positioning had synergy with the existing standard of care. But, the client was also eager to learn how that treatment conversation would change with the addition of their product.
We could easily have relied on technology and applications to learn about the treatment conversations, or even pursued other ways of simulating the conversation, such as virtual reality. However, we felt strongly that to really understand the human interaction between physician and patient, we needed a methodology that would allow us to fully explore both the rational and emotional dynamics of the conversation.
The Preparation
Much like actual theater performance, all the hard work happens behind the scenes with role-play. Leveraging our foundational patient research and deep knowledge of the disease state, we developed our scenarios and our patient personas. The actors that we cast to portray our patients were provided with more than a medical history—they were given in-depth lifestyle and family background, emotional character development, and specific context about their disease (how they came to be diagnosed, their reaction in that moment, their underlying fears about the disease). We work to ensure that when these actors enter the simulation with a physician, they are prepared to behave, speak and emote as realistically as possible.
We know physicians will tailor their dialogue and explanations based on the patient’s needs and personality, so we prepared two different patient types that we came to understand in our patient research:
- “Joe”: A blue-collar, semi-retired male who lived with his wife, he hates going to the doctor unless he really has to. He’s had a few health problems, but relies on his doctor to tell him what to do. His wife does have to remind him to take care of himself, and he only got himself checked out because she pushed him—and then he found it wasn’t just a cough; it was cancer.
- “Madelyn”: A hard-working, ambitious corporate professional who puts all of her effort into her work. She’s never had any health issues before, but after a car accident, she had scans done in the ER and her cancer was discovered. She immediately went into action mode, reading everything she could and trying to figure out what her best options would be.
The Creative Approach
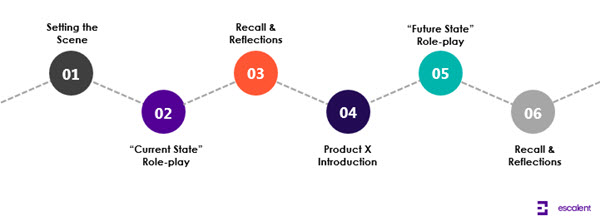
For the research engagement, we prepared physicians at the recruitment phase to expect role-play as part of their participation in the research. The discussion began with a brief discussion of their practice, the challenges of treating this tumor type, and then setting the scene for the first role-play by providing a patient chart and explaining that this was their first consult with Joe or Madelyn, where they would be reviewing the treatment plan. After observing the conversation, we debriefed with the physicians to understand why they chose a certain language or made certain decisions. Then, we showed a product profile and asked them to engage in a second role-play—this time in the hypothetical future when “Product X” was available. Again, our patient came in, and the physicians engaged in the simulated “future state” conversation, followed by another debrief before the interview closed.
The Outcomes
After conducting these role-play simulations in markets across the US, we discovered that by examining the dialogue of these conversations we were also revealing key emotional learnings and valuable product insights. Our human approach took us beyond the conversation and into the unmet needs within this tumor setting, and helped us understand what was most important to physicians through what they shared with our patient actors.
The unexpected and beneficial outcomes of the research included…
- Direction for brand positioning territories: While physicians expressed receptivity to Product X, it was the observation of how expectations were framed to patients compared to the current treatment paradigm that revealed unmet needs and underlying physician tensions—creating paths to the brand’s positioning.
- Language to inform brand messaging to HCPs: Our detailed analysis of language and dialogue revealed valuable words, phrases and metaphors that directly informed message development.
- Insight for disease state and patient messaging: By listening and collecting the various terminology, analogies and explanations provided by the HCPs to the patient actors, the marketing team effectively built upon and employed these “tried and true” strategies in their campaign development.
Director’s notes
In employing role-play as a health research methodology, we have a few notes from the director’s chair to help ensure success…
- Remember, it’s improv, not Broadway: It’s important to know that we did not give our patient actors a script to follow. That type of formulaic approach would have dampened the human aspect of our approach. Part of why our physicians were able to engage in the simulation is because the actors behaved like real patients—depending on the patients’ character, they deferred or challenged, they emoted or withheld, and they interrupted the doctor with hard questions. Each engagement in the research was different, as the actors reacted to the different language and approach the doctor took—they read and reacted to the doctor as a person, too, which is why we got closer to reality than other simulation exercises.
- Learn, iterate and adapt: When we discovered in our introduction with a physician that he or she had a certain perspective or approach, we gave quick guidance to our actors to explore that feature somehow—prompting with a question or reacting emotionally to a specific phrase. One of the advantages of role-play is the ability to manipulate variables to understand how they influence dialogue, language or decision-making.
- Preparation is everything: To prepare our actors, we had to deeply understand the patient experience, which required quality foundational research. It was only through real patient experiences and emotions that we were able to fully develop characters for these scenarios. Equally as important was preparation for our physician respondents—making them aware of the role-play in advance, providing any tools or materials they might need during the scenario, and creating an environment that feels natural to them (an exam room or office).
- Consider the other influences in conversations: If decision-making is critical to the research objectives, it is essential to consider “who else” might need to be involved in the simulation. Are caregivers present? We may consider preparing caregiver actors to join our patients. Do different specialists work together to present the treatment plan? We may recruit both specialists and give them time to discuss the case before bringing the patient actor in. We work to be as thorough as possible in simulating all of the appropriate variables in order to learn effectively.
At Escalent, we are relentless in finding creative ways to access real-world human insights, even when the behaviors and decisions that we are after happen behind closed doors. Role-play is just one of our ways behind those doors—send us a note if you would like to talk about the creative ways we can help uncover your next human insights.








